Although 1 in 5 men and 1 in 6 women worldwide develop some type of cancer during their lifetime, those diagnosed are living longer than ever, thanks to screening and early detection, vaccinations, and improvements in treatment. However, even for cancers with effective treatment options, prevention has the greatest potential to reduce the burden of cancer in the general population. [1]
Because each person is exposed to unique environmental and lifestyle factors, cancer risk can vary. Although some factors cannot be controlled (such as inherited genetic mutations), there is a range of modifiable environmental and lifestyle factors that can help reduce the risk of developing cancer.
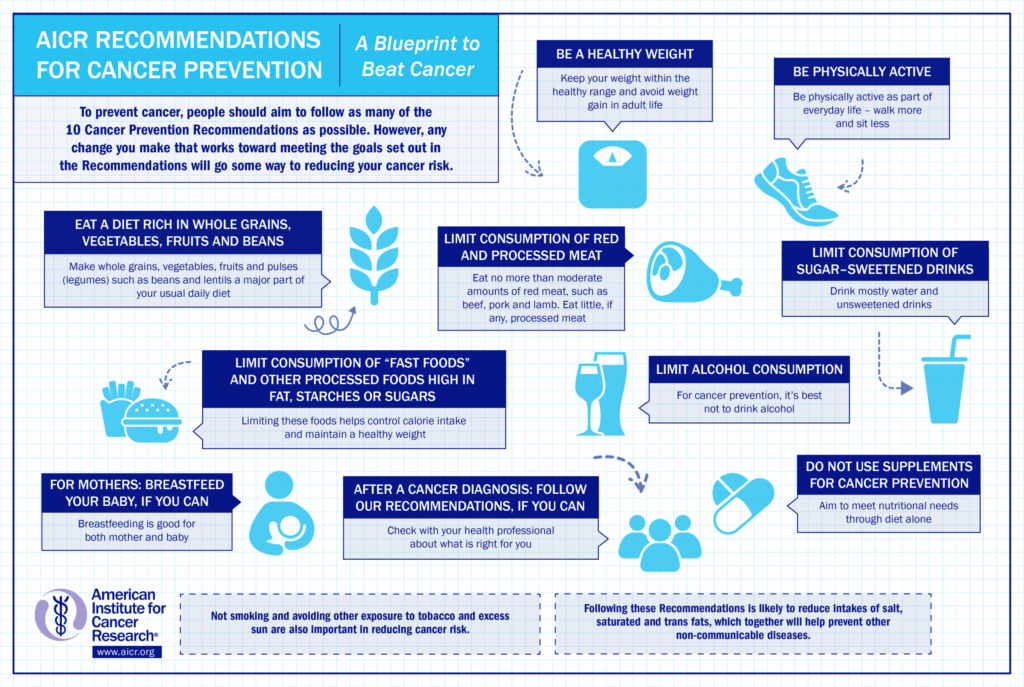
According to the World Health Organization (WHO), a 30-40% cancer burden can be attributed to lifestyle risk factors such as tobacco smoking, alcohol consumption, a diet low in fruit and vegetables, overweight and obesity, and physical inactivity. [2] In a 2018 report by the World Cancer Research Fund (WCRF) and the American Institute of Cancer Research (AICR), not-for-profit organizations that lead a network of cancer prevention charities with a global reach, 10 cancer prevention recommendations on diet and nutrition were developed. These recommendations were based on the continuous update project of evidence in cancer research, which summarizes current evidence with relevant papers from randomized controlled trials and cohort studies. [3] Taken together, they promote a lifestyle consisting of a healthy dietary pattern, physical activity, and weight management. This may not only help reduce the risk of cancer but may also contribute to the prevention of obesity and other chronic diseases such as type 2 diabetes and cardiovascular disease.
Here is a closer look at some of their recommendations:
Maintain a Healthy Weight
In a meta-analysis conducted by the WCRF/AICR, there is convincing evidence that carrying extra fat mass, marked by a higher body mass index (BMI), greater waist circumference, and greater waist-to-hip ratio, significantly increases the risk of several cancers: [4]
- BMI measures one’s weight in relation to height. A BMI between 18.5-25 is classified as normal, 25.1-29.9 overweight, and 30 or higher obese. Each increase of 5 points in BMI was associated with a 50% higher risk of endometrial cancer, 48% higher risk of esophageal adenocarcinoma, 30% higher risk of kidney cancer, 30% higher risk of liver cancer, 12% higher risk for postmenopausal breast cancer, 10% higher risk of pancreatic cancer, and 5% higher risk of colorectal cancer.
- Each 4-inch increase in waist circumference was shown to increase the risk of esophageal adenocarcinoma by 34%, pancreatic cancer by 11%, postmenopausal breast cancer by 11%, kidney cancer by 11%, endometrial cancer by 5%, and colorectal cancer by 2%.
- A waist-to-hip ratio (WHR) measures one’s waist size divided by hip size. People who carry more weight in the belly (apple shape) are at higher risk for cancer and other chronic diseases than those who carry more weight in the hips (pear shape). The WHO recommends a healthy WHR to be 0.9 or less in men and 0.85 or less in women. Each 0.1 unit increase in waist-hip ratio significantly increased the risk of esophageal adenocarcinoma by 38%, kidney cancer by 26%, endometrial cancer by 21%, pancreatic cancer by 19%, postmenopausal breast cancer by 10%, and colorectal cancer by 2%.
Significant increasing weight in adult life is a convincing cause of postmenopausal breast cancer and endometrial cancer.
- Each 11-pound increase in weight gain during adulthood was significantly associated with a 16% higher risk of endometrial cancer, and 6% higher risk of postmenopausal breast cancer.
Incidence of obesity-related cancers is also rising in young adults. Researchers from the American Cancer Society collected data from 25 state cancer registries for people ages 25-84 years diagnosed with any cancer from 1995 to 2014. [5] Over this time period, incidence rates of several obesity-related cancers—including colorectal, kidney, and pancreatic—increased significantly in the youngest age group, ages 25-49 years (with the sharpest increases in progressively younger ages). Although the incidence of these cancers also rose in older age groups, the rate of increase was much smaller.
Be Physically Active
Physical activity is defined as any movement that uses skeletal muscles and requires more energy than does resting. Physical activity can include working, exercising, performing household chores, and leisure-time activities such as walking, jogging, running, yoga, hiking, bicycling, and swimming.
There is evidence from a 2009 meta-analysis of 52 epidemiologic studies showing that the most physically active individuals had a 24% lower risk of colon cancer than those who were the least physically active. [6] A 2013 meta-analysis of 31 prospective studies showed that the average breast cancer risk reduction associated with physical activity was 12%, and the protective effect was stronger for postmenopausal women. [7] After menopause, women who increase their physical activity may also have a lower risk of breast cancer than women who do not. [8]
Sedentary behaviors, such as spending an extended amount of time sitting, reclining, or lying down, may also increase cancer risk. [9] The review of research on sedentary behavior and risk of endometrial, colon, and lung cancers found that the highest versus lowest levels of sedentary time increased risks of these cancers by a statistically significant range of 20-35%. [10]
Eat a Healthful Diet

An overall healthy dietary pattern has the potential to lower cancer risk by 10-20%. [11] The association between diet and cancer incidence varies by cancer sites and also by sex, [12] but the recommended components of a healthy diet are often similar. The WCRF/AICR listed the following dietary recommendations to protect against cancer:
- Limit alcohol consumption. [13] There is strong evidence that consumption of alcoholic drinks is a cause of cancers of the mouth, pharynx and larynx, esophagus (squamous cell carcinoma), liver, colorectum, and breast (particularly postmenopause). Every 10 grams of alcohol (as ethanol) consumed per day elevated the risks of these cancers by 4-25%. The evidence shows that alcoholic drinks of all types have a similar impact on cancer risk. This recommendation therefore covers all types of alcoholic drinks, whether beer, wine, spirits (liquors), or any other alcoholic drinks, as well as other alcohol sources.
- Eat a diet rich in whole grains, vegetables, fruit, and beans. [14] Make whole grains, vegetables, fruit, and pulses (legumes) such as beans and lentils a major part of your daily diet. There is strong evidence that eating whole grains protects against colorectal cancer, and that eating foods containing dietary fiber protects against colorectal cancer, weight gain, overweight, and obesity, which, as described above, increases the risk of many cancers.
- Limit “fast” foods. [15] Fast foods are readily available convenience foods that tend to be energy-dense and are often consumed in large portions. Most of the evidence on fast foods is from studies looking at burgers, fried chicken, French fries, and high-calorie drinks (containing sugar, such as soda; or unhealthy fats, such as shakes). There is strong evidence that diets containing higher amounts of fast foods and other processed foods high in unhealthy fats, starches, or sugars, as well as consuming a “Western type” diet (characterized by a high amount of added sugars, meat, and fat), are causes of weight gain, overweight, and obesity, which are a risk factor for many cancers.
- Limit red and processed meat. [16,17] Red meat includes all types of muscle meat from a mammal, including beef, veal, pork, lamb, mutton, horse, and goat. Processed meat has been transformed through salting, curing, fermentation, smoking, or other processes to enhance flavor or improve preservation. Although these products are often made from red meat (i.e., ham, salami, bacon, and some sausages such as frankfurters and chorizo), other meats can also be processed (i.e., turkey bacon, chicken sausage, and deli-sliced chicken). While both red and processed meat were suggested to increase the risk of a number of other cancers, the evidence was most convincing for colorectal cancer. The risk of colorectal cancer increased by 16% with every 50g/day of processed meat intake, and by 12% with every 100g/day of red meat intake. Because meat can be a valuable source of nutrients, in particular protein, iron, zinc, and vitamin B12, the recommendation is to limit rather than completely avoid minimally processed red meat. However, poultry and seafood are generally healthier sources of protein as well as many of these other nutrients. Very little, if any, processed meat should be consumed.
- Limit sugar-sweetened drinks. [18] There is convincing evidence that sugar-sweetened drinks is a cause of weight gain, overweight, and obesity in both children and adults, especially when consumed frequently or in large portions. As noted above, obesity increases the risk of many cancers.
Avoid Tobacco and Excess Sun Exposure
The recommendations also emphasize that not smoking and avoiding other exposure to tobacco and excess sun are also important in reducing cancer risk.
Cancer survivorship
With improved early detection and availability of more advanced treatment options, people diagnosed with cancer are living much longer. Research on the effects of diet, nutrition, and physical activity on the risk of cancer in cancer survivors is growing, but much more limited than that on risk. Therefore, the lifestyle recommendations mentioned above emphasize that all cancer survivors should receive nutritional care and physical activity guidance from trained professionals.
Although evidence is not strong enough to reach firm conclusions, there are indications of links between lifestyle factors and cancer survivorship with improved quality of life and longer survival, especially for more common cancers. For example, maintaining a healthy weight, being physically active, eating foods containing fiber, and having a lower intake of saturated fat appear to lead to better survival after a breast cancer diagnosis.[14] Unless otherwise advised, and if they can, all cancer patients and survivors are advised to follow the WCRF/AICR Cancer Prevention Recommendations as long as possible after the acute stage of treatment.
These recommendations are also helpful for managing or preventing other chronic diseases after a cancer diagnosis. A study of survivors of the 20 most common cancers revealed that, even after controlling for the overlapped risk factors for cancer and cardiovascular disease such as excessive weight and smoking, survivors of most site-specific cancers had an increased risk for cardiovascular diseases compared with that of the general population. [15] Evidence has shown that certain cancer treatments, for example anthracycline and trastuzumab, can lead to a higher risk of disease and death from cardiovascular complications. [16-18]
Related
- Cancer: Overview, Types, and Risk Factors
- Prevention Information and Cancer Fact Finder Tool from the Zhu Family Center for Global Cancer Prevention at the Harvard Chan School of Public Health
Last reviewed March 2021